Medicare Appeals
By Kellie Mattos, C.A.C.
How to be a WINNER with Medicare appeals.
Medicare appeals can be time-consuming and tedious with, frequently, no positive outcome for your effort. Today I am going to talk about the importance of appeals and how to win them!
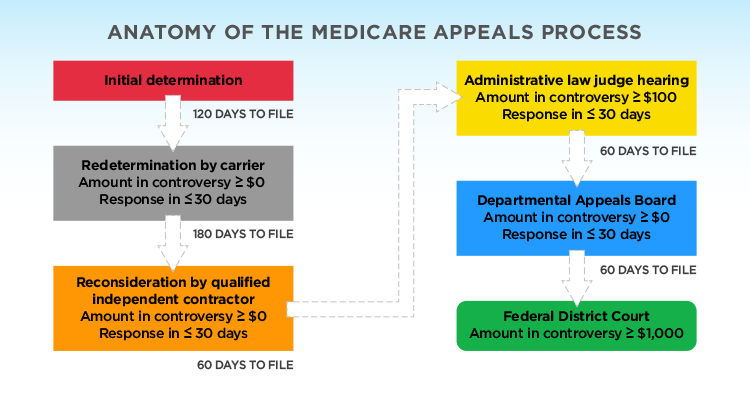
Anatomy of an Appeal- Time Consuming and Tedious
When a claim is first submitted to Medicare the claim is delivered electronically and is not actually reviewed by a person. The denial is usually caused by a pre-programmed algorithm set to deny a part(s) of your claim that it believes shouldn’t be paid, for one of unlimited reasons.
Now is the time to appeal for what’s rightfully owed to you!
Level One: Denied – First Appeal
A first-level appeal to Medicare is reviewed by a Medicare Administrative Contractor (MAC) staff member. This is the first chance to defend the claim by submitting not only the trip reports, medical necessity forms and hospital records, but also present the Medicare rules and regulations that pertain to the specific area(s) of the denial. If you are able to cite the CMS rules and regulations specifically, this creates a better chance of winning the appeal because you are now providing both the documentation and proof that the claim should not have been denied in the first place.
An Example Scenario: The Denial
A specialized ventilated patient who also requires hemodialysis services and is being transported to a skilled nursing facility.
Not many facilities accept these patients, requiring the patient to be transported outside of the normal locality area. It should be noted here that Medicare automatically denies ground transports with a loaded mileage charge greater than 250 miles. However, if the skilled rehabilitation facility is the most appropriate for your patient then initiating an appeal is appropriate.
Properly filing an appeal for this claim will necessitate completing a detailed summary outlining the patient’s need for an ambulance transport to the destination facility. This is a good place to cite the Medicare Manual Chapter 10 Section 10.3.6 as reference that the destination is in fact the most “appropriate” facility for that particular patient. (this section also provides direct reference when appealing denials received for transports involving scenarios such as when closer beds are not available, because as we all know some facilities fill to capacity limitations quickly.)
Level Two: Denied Again- Second Appeal
If the first appeal was denied upon review and yet you continue to feel strongly about the validity of the claim then move on- file that second level appeal!
Second appeals are hosted by a third-party arbitrator that are independent from the MAC’s review. These appeals are initiated by filing with the Qualified Independent Contractor (QIC) for your area. Filing with the QIC will enable you to have a fresh set of eyes, independent of the MAC, to view all of your documents in support of your appeal argument.
In the end, should the QIC overturn MAC’s denial then you will receive the payment!
MA-130? Don’t give up!
MA-130 denial code means the claim contains incomplete and/or invalid information, and no appeal rights are afforded because the claim is unprocessable.
Don’t give up just yet! Oftentimes these trips can be revised and resubmitted to produce a clean claim. First, read over the entire remittance notifying you of the denial to see if the other denial codes listed can help to define what exactly made this claim not payable (and not able to be appealed in its present form). If you’re stuck, ask someone to take a look at the claim together with you. We find that a fresh set of eyes can help, so don’t hesitate to reach out for assistance. Medicare can be difficult to navigate but if you follow their rules you can beat them!
Can’t win them all
Unfortunately, there is never a guarantee you will win any of the appeals, but with careful thorough documentation and perseverance, the odds can always be in your favor, just like they are for us here in our QMC billing office!
Good luck with your appeals!
Kellie has been with Quick Med Claims for 11 years and is an account manager support supervisor with her CAC.
